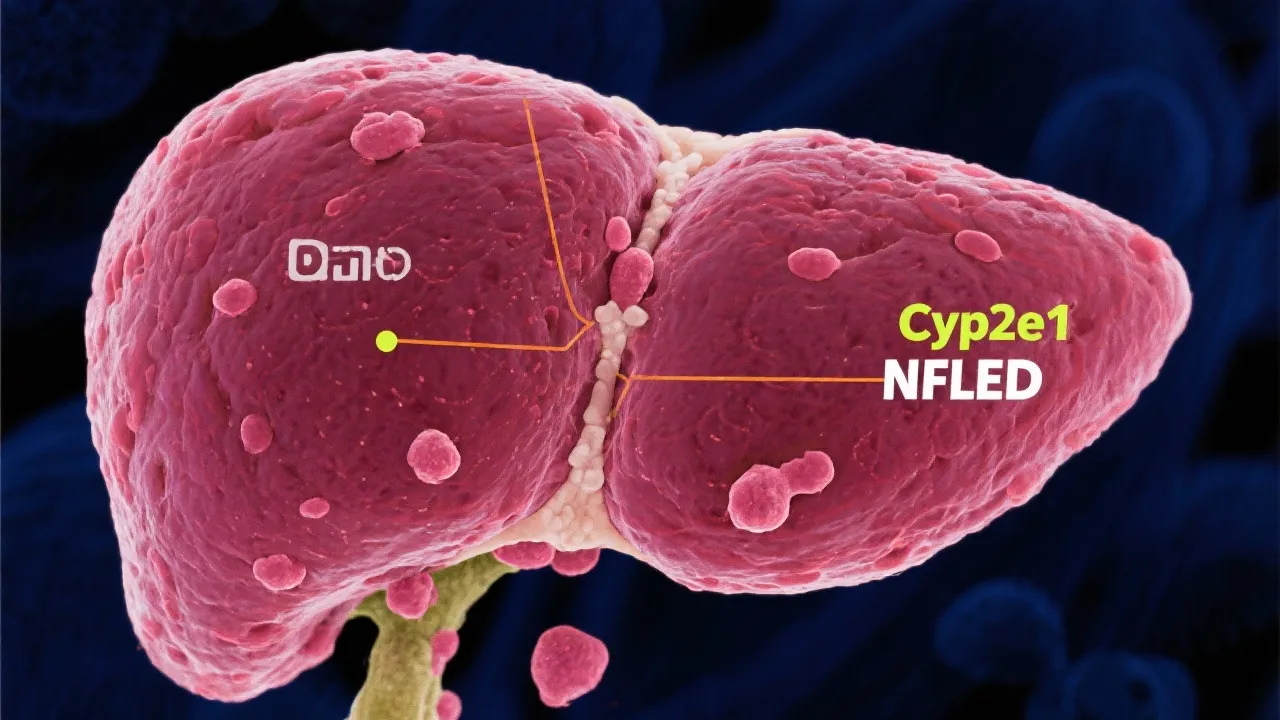
Role of Cyp2e1 in NAFLD
This article explores the intricate relationship between Cyp2e1 and Non-Alcoholic Fatty Liver Disease (NAFLD). Cyp2e1, an enzyme involved in drug metabolism, has been studied for its potential impact on liver diseases like NAFLD. Understanding this enzyme's role can enhance insights into the pathogenesis and progression of NAFLD, offering avenues for targeted therapeutic strategies.
Introduction to Cyp2e1 and NAFLD
Non-Alcoholic Fatty Liver Disease (NAFLD) is a prevalent condition affecting millions worldwide, characterized by excessive fat accumulation in the liver without significant alcohol consumption. The cytochrome P450 2E1 (Cyp2e1) enzyme is a crucial player in the metabolism of various substances and has garnered attention for its role in the pathogenesis of NAFLD. This article delves into how Cyp2e1 influences NAFLD, its potential impact on liver health, and the implications for treatment strategies.
Understanding Cyp2e1 and Its Functions
Cyp2e1 is part of the cytochrome P450 superfamily, enzymes responsible for the oxidative metabolism of several xenobiotics and endogenous substrates. This enzyme is primarily expressed in the liver, where it participates in the bioactivation of small, hydrophobic molecules. The reactive oxygen species (ROS) generated during this metabolic process can induce oxidative stress, a well-established factor in the progression of liver diseases, including NAFLD. To fully understand the intricacies of Cyp2e1, it is crucial to explore its substrate specificity, regulation, and the downstream effects of ROS on liver function.
The expression of Cyp2e1 is modulated by various factors, including dietary components, environmental toxins, and underlying metabolic conditions such as obesity and diabetes. This enzyme's activity can escalate significantly under pathological circumstances, notably reinforcing the cycle of tissue damage and inflammation that characterizes NAFLD.
Overall, Cyp2e1 plays a dual role: while it is essential for the detoxification of harmful substances, its overactivity can lead to significant pathological consequences, particularly in the context of metabolic dysregulation.
Linking Cyp2e1 to NAFLD Pathogenesis
Research suggests that elevated levels of Cyp2e1 contribute to the oxidative stress observed in NAFLD. NAFLD progression, from simple steatosis to non-alcoholic steatohepatitis (NASH), involves inflammation and hepatocellular injury exacerbated by oxidative stress. Cyp2e1 not only enhances lipid peroxidation but also affects the integrity of cellular membranes, facilitating the advancement of liver damage. The mechanistic insight into how Cyp2e1 influences these pathological processes is crucial for establishing effective therapeutic measures.
Studies have indicated that Cyp2e1 activation leads to the generation of toxic metabolites that can directly damage hepatocytes. These metabolites can induce apoptosis—a programmed cell death process that further aggravates liver inflammation. Chronic activation of Cyp2e1 aligns with the development of liver fibrosis, wherein excessive scar tissue builds up due to ongoing liver injury and inflammation. This progression toward fibrosis correlates with an increased risk of cirrhosis and hepatocellular carcinoma, highlighting the critical role of Cyp2e1 in liver disease severity.
| Mechanism | Impact on NAFLD |
|---|---|
| Oxidative Stress | Cyp2e1 elevates oxidative stress, furthering liver inflammation and damage. |
| Lipid Peroxidation | Increased lipid peroxidation augments liver fibrosis, advancing NAFLD severity. |
| Inflammatory Response | Cyp2e1 influences cytokine production, promoting inflammatory pathways in NAFLD. |
| Cellular Apoptosis | Release of reactive metabolites leads to apoptosis of hepatocytes, worsening liver health. |
Innovative Approaches to Address Cyp2e1 Activity in NAFLD
Given the detrimental effects of Cyp2e1 in NAFLD progression, targeting this enzyme may offer therapeutic benefits. Several strategies are under exploration, including the development of inhibitors that specifically modulate Cyp2e1 activity. Antioxidants that mitigate oxidative stress and lifestyle modifications such as dietary supplementation with polyunsaturated fatty acids may also help in reducing Cyp2e1-mediated liver damage. The integration of these strategies could pave the way for a multifaceted approach in managing NAFLD.
One promising avenue involves the use of pharmacological inhibitors that selectively inhibit Cyp2e1 activity. Compounds like diallyl sulfide, found in garlic, and other natural products have shown potential in preclinical models for their ability to reduce oxidative stress and inflammation mediated by Cyp2e1. Additionally, research is evaluating the effectiveness of novel synthetic inhibitors designed to target Cyp2e1 while minimizing adverse effects on other metabolic pathways.
Furthermore, lifestyle interventions, particularly diet and exercise, play a significant role in modulating the activity of Cyp2e1. A diet rich in omega-3 fatty acids can downregulate the expression of Cyp2e1, possibly due to the anti-inflammatory properties associated with these fats. Regular physical activity can also enhance metabolic health and, in turn, may mitigate the risks of NAFLD-associated Cyp2e1 overactivity, highlighting the importance of holistic approaches to managing liver health.
Future Research and Management Implications
Further research is necessary to elucidate the precise mechanisms by which Cyp2e1 contributes to NAFLD. Clinical trials focusing on Cyp2e1 inhibitors and their efficacy in preventing or reversing NAFLD progression could reshape treatment paradigms. Additionally, integrating genetic analyses into routine diagnostics might help identify individuals at a higher risk of Cyp2e1-associated liver damage, allowing for personalized intervention strategies tailored to individual risk profiles.
Emerging techniques such as CRISPR-Cas9 gene editing are showing potential in studying gene function related to Cyp2e1. By knocking down or modifying specific genes involved in the expression and regulation of Cyp2e1, researchers can further pinpoint the enzyme's role in metabolic disease pathways. This could lead to novel therapeutic targets that can be exploited to halt or even reverse NAFLD progression.
Moreover, understanding the hepatic metabolomics associated with Cyp2e1 activity could provide insights into biomarker development for early diagnosis and treatment response tracking. Identifying specific metabolic signatures associated with Cyp2e1-mediated lipotoxicity may enhance our capacity to predict the trajectory of NAFLD in individuals with varying degrees of liver disease severity.
Comparing Cyp2e1 and Other Cytochrome P450 Enzymes in NAFLD
While Cyp2e1 has been highlighted for its detrimental roles in NAFLD, it is essential to consider its functional interplay with other cytochrome P450 enzymes such as Cyp1A2 and Cyp3A4, which also play roles in drug metabolism and the oxidative stress response in the liver. For instance, while Cyp2e1 predominantly catalyzes the metabolism of ethanol, its activity can influence the expression and activity of other P450 enzymes in parallel, compounding the effects of oxidative stress in fatty liver disease.
Cyp1A2, for example, is considered less actively involved in lipid metabolism but has been implicated in the bioactivation of pro-carcinogenic compounds. Similarly, Cyp3A4, the most abundant P450 enzyme in the liver, interacts with various drugs and endogenous compounds that can influence liver health. Understanding the comparative roles and regulatory mechanisms of these enzymes can provide a more nuanced view of the liver’s response to stressors, potentially identifying new domains for intervention.
Impact of Comorbidities on Cyp2e1 Activity in NAFLD
NAFLD typically presents alongside a range of comorbidities including obesity, type 2 diabetes, and cardiovascular disease. The presence of these conditions can significantly modulate Cyp2e1 activity, elevating the risk of liver damage. In states of obesity and insulin resistance, there is an augmented release of free fatty acids, which can stimulate the overexpression of Cyp2e1. This further exacerbates the oxidative damage and inflammatory response in the liver.
Also, comorbidities can influence the pharmacokinetics and pharmacodynamics of medications used to treat NAFLD. Understanding how Cyp2e1 interacts with commonly prescribed medications for type 2 diabetes or hyperlipidemia is crucial for optimizing treatment regimens and avoiding potential drug-induced hepatotoxicity.
FAQs
- What is the primary function of Cyp2e1?
Cyp2e1 primarily facilitates the oxidative metabolism of a wide range of xenobiotics and endogenous compounds, contributing to the production of reactive oxygen species.
- How does Cyp2e1 affect liver health in NAFLD?
Through increased oxidative stress and lipid peroxidation, Cyp2e1 exacerbates liver inflammation, fibrosis, and overall damage, worsening NAFLD.
- What potential treatments exist for targeting Cyp2e1 in NAFLD?
Research is underway on Cyp2e1 inhibitors, along with the use of antioxidants and lifestyle changes to manage oxidative stress and liver inflammation.
- How does obesity impact Cyp2e1's role in liver disease?
Obesity can enhance the expression and activity of Cyp2e1, leading to increased oxidative stress and inflammation in the liver, worsening NAFLD.
- Are there specific dietary changes that can lower Cyp2e1 activity?
A diet rich in antioxidants and omega-3 fatty acids may help modulate Cyp2e1 activity, reducing oxidative stress and liver inflammation associated with NAFLD.
Conclusions
Understanding the role of Cyp2e1 in NAFLD provides valuable insights into the disease's complexity and progression. With ongoing research focused on this enzyme, future therapeutic interventions could play a significant role in combating the global burden of NAFLD, improving patient outcomes through targeted and personalized medical strategies. An interdisciplinary approach that combines molecular biology, pharmacology, and lifestyle interventions might pave the way for innovative solutions to effectively manage and potentially reverse the impacts of NAFLD, elevating the standard of care for individuals affected by this multifaceted condition.