Understanding Seimc Hepatitis
Seimc Hepatitis is a significant condition affecting liver health. The term "Seimc Hepatitis" might not be widely recognized in existing medical literature, but it likely pertains to a specific subset of hepatitis, an inflammation of the liver. Hepatitis has various causes including viral infections, autoimmune diseases, or exposure to certain medications. This article explores the intricacies of Seimc Hepatitis, analyzing its implications and treatment approaches.

Introduction to Liver Health
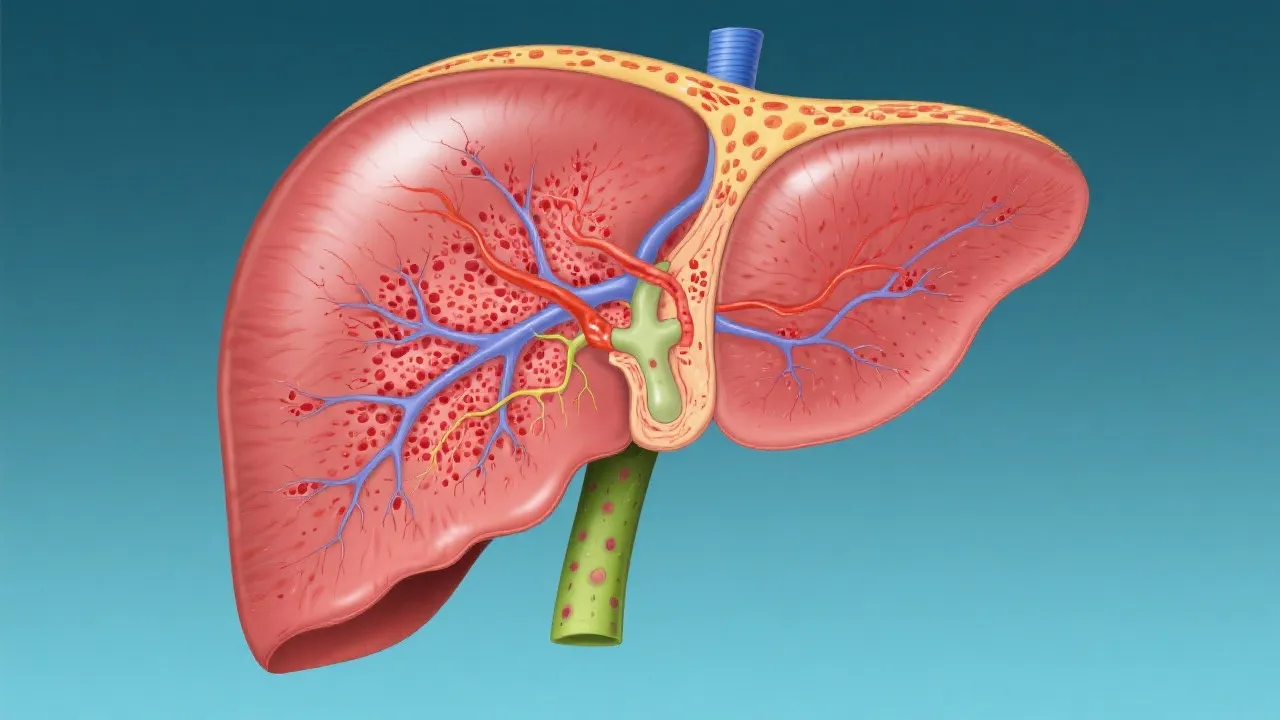
The liver is a vital organ responsible for numerous essential functions, including metabolism regulation, detoxification, and the production of biochemicals necessary for digestion. It's the body's largest internal organ and plays a crucial role in several bodily functions, which include but are not limited to bile production, nutrient metabolism, and the synthesis of proteins necessary for blood clotting. Maintaining liver health is crucial for overall well-being, and any impairment can lead to significant health issues.
Additionally, the liver processes everything we eat and drink, filtering toxins from the blood, regulating blood sugar levels, and providing the body with energy. Beyond these physical functions, the liver also plays a role in hormone regulation and immune function, making it an essential component of our overall health. An unhealthy liver can lead to a myriad of problems, from liver disease and failure to increased risk of infections and complications in other bodily systems.
Understanding liver health is critical not just for those who may be at risk due to lifestyle choices or genetic predispositions, but also for anyone interested in optimizing their health. Regular check-ups and relevant blood tests can help in monitoring liver function, enabling proactive measures to be taken if any issues are detected.
Defining Seimc Hepatitis
Seimc Hepatitis is a term that might not be prevalent in mainstream medical terminology. Still, it is essential to understand its context within the broader category of hepatitis. Generally, hepatitis refers to the inflammation of the liver, and this can stem from a multitude of factors including viral infections, such as Hepatitis A, B, and C, or autoimmune responses, drugs, and alcohol consumption. The term 'seimc' possibly denotes a specific or less recognized form of hepatitis that is characterized by particular symptoms, laboratory findings, or epidemiological features.
In understanding this condition, it’s important to draw clear distinctions between the terminologies used in liver diseases. Various forms of hepatitis are defined based on their causes, pathogenesis, clinical features, and possible outcomes. For instance, while we commonly hear about viral hepatitis in the context of epidemics or high-risk populations, there are also less common forms of hepatitis which may be referred to using broader or even regional terminologies. Recognizing the subtleties in these diseases can aid in appropriate identification and management.
Causes and Risk Factors
The root causes of hepatitis vary depending on its type. Viral hepatitis, caused by different viruses, is among the very common forms. Non-infectious causes might include prolonged alcohol use, exposure to toxic substances, or autoimmune diseases where the body mistakenly attacks healthy liver cells. Among the viral types, hepatitis A, B, C, D, and E are the most recognized, each having unique modes of transmission and epidemiological profiles.
Hepatitis A virus (HAV) is commonly transmitted via ingestion of contaminated food and water, often in regions with poor sanitation. Hepatitis B (HBV) can be transmitted through contact with infectious body fluids, which raises concerns in the context of unsafe sexual practices and sharing needles. Similar to HBV, the Hepatitis C virus (HCV) is also primarily transmitted through blood-to-blood contact, making it particularly concerning in healthcare settings and among intravenous drug users.
Additional risk factors enhancing susceptibility to hepatitis include age, as older adults may have weaker immune responses; certain chronic medical conditions, such as diabetes and obesity, which can predispose individuals to liver conditions; and lifestyle factors including alcohol consumption and illegal substance use. It’s imperative to understand how lifestyle choices can interact with genetic predispositions to create varying levels of risk for developing liver illnesses.
Symptoms and Diagnosis
Common symptoms of hepatitis include jaundice (yellowing of the skin and eyes), fatigue, abdominal pain, nausea, fever, and loss of appetite. Other symptoms can manifest depending on the severity and specific type of hepatitis, which can sometimes make diagnosis tricky at the onset since they may closely resemble flu-like symptoms. Chronic cases may result in more severe symptoms, such as dark urine, clay-colored stools, and severe abdominal swelling.
To diagnose hepatitis, healthcare providers typically rely on a combination of physical examinations, blood tests, imaging studies like ultrasound, and liver biopsies to assess the extent of liver inflammation and function. Blood tests can reveal elevated liver enzyme levels—an indicator of inflammation or damage to liver cells—and help in determining which specific type of hepatitis is present. For example, serological tests can distinguish between past infections and current active hepatitis.
Differentiating among the types of hepatitis can influence treatment strategies and management approaches. Imaging studies such as ultrasound or CT scans can provide additional insights, revealing abnormalities in liver size or structure, while liver biopsies allow for direct examination of liver tissue, which can clarify the extent of damage or inflammation present.
Treatment Options
Treatment plans for hepatitis vary based on its cause. In cases of viral hepatitis, antiviral medications can reduce the viral load and promote liver recovery. For example, newer direct-acting antiviral medications available for Hepatitis C have shown promising success rates for curing the infection and halting liver disease progression. Lifestyle changes play a critical role, including reducing alcohol intake and following a liver-friendly diet rich in fruits, vegetables, whole grains, and lean proteins.
In cases where autoimmune causes are identified, immunosuppressive drugs may be prescribed to manage the immune system’s response. This tailored approach is crucial as autoimmune hepatitis may require long-term management to prevent further damage to the liver. It is also important for individuals with chronic liver conditions to engage in regular monitoring and follow-up appointments with their healthcare providers.
For advanced liver disease or cirrhosis, where the liver has sustained significant damage, more invasive treatments such as liver transplantation may be considered. This option is typically reserved for severe cases where liver function is critically impaired. Additionally, holistic approaches incorporating mental health support, nutritional counseling, and exercise regimens may assist patients in achieving better health outcomes and improving their quality of life.
Comparative Analysis of Hepatitis Types
| Type of Hepatitis | Cause | Treatment Approach |
|---|---|---|
| Hepatitis A | Caused by Hepatitis A virus; often spread through contaminated food or water. | Generally resolves on its own; preventive vaccination available. |
| Hepatitis B | Caused by Hepatitis B virus; spread through blood, semen, or other body fluids. | Antiviral medications and monitoring; vaccination available for prevention. |
| Hepatitis C | Caused by Hepatitis C virus; primarily spread through blood contact. | Antiviral treatment leading to cure in many cases; no vaccine available. |
| Hepatitis D | Requires the presence of Hepatitis B virus; typically spreads through contact with infectious body fluids. | No specific treatment; managing Hepatitis B may reduce severity. |
| Hepatitis E | Caused by Hepatitis E virus; often spread through contaminated water, particularly in regions with poor sanitation. | Treatment focuses on hydration; vaccination available in some countries. |
| Autoimmune Hepatitis | Unknown cause; thought to involve genetic predisposition and environmental factors. | Immunosuppressive medications aimed at reducing immune response. |
Prevention Strategies
Preventive measures vary based on the type of hepatitis. For viral forms, vaccinations (particularly for Hepatitis A and B) are highly recommended. Hepatitis A vaccines are especially crucial for travelers to endemic regions, while Hepatitis B vaccinations are universally advised as part of routine immunizations for infants and at-risk adults. Hygiene practices, including proper hand washing and safe food handling, are essential to preventing Hepatitis A transmission.
Safe sexual conduct and education on the risks associated with sharing needles or equipment can assist in preventing the spread of Hepatitis B and C. It is vital for individuals with risk factors to engage in regular screening and testing to catch infections early, reducing the potential for complications and spread to others.
In addition, public health initiatives promoting screening and education about liver health can cultivate a more informed population capable of making healthier choices concerning their liver and overall well-being. These strategies can reduce the incidence of liver-related diseases, emphasizing the critical need for awareness and education in the proper management of hepatologic health.
FAQs
- What is the main difference between viral and autoimmune hepatitis? Viral hepatitis is caused by infections from the hepatitis viruses, while autoimmune hepatitis occurs when the immune system mistakenly attacks healthy liver cells, leading to inflammation and damage.
- How is hepatitis diagnosed? Diagnosis involves comprehensive blood tests to check liver enzyme levels, serological markers for viral infections, alongside liver function tests, and possibly imaging or biopsy to assess liver damage.
- Can lifestyle changes improve liver health? Yes, adopting a healthy lifestyle, including a balanced diet rich in antioxidants, regular exercise, limiting alcohol intake, and managing weight can significantly improve liver function and health.
- What dietary choices can support liver health? Including foods rich in omega-3 fatty acids, fiber, and vitamins A, C, and E can enhance liver function. Leafy greens, cruciferous vegetables, and fresh fruits are also beneficial.
- Is liver disease reversible? Depending on the stage and cause of liver disease, early intervention and lifestyle changes may reverse some liver damage. For instance, fatty liver disease can often be improved with significant lifestyle modifications.
- What regular tests should I have for liver health? Routine liver function tests, ultrasound screening, and for those at risk, hepatitis screenings should be done regularly. Consult your healthcare provider for personalized recommendations.
Conclusion
Maintaining liver health is essential for ensuring our overall health and longevity. By understanding the causes and implications of various forms of hepatitis, individuals can take proactive steps towards prevention, early detection, and effective treatment. Awareness and education about liver health can empower people to make informed choices regarding their lifestyles and healthcare decisions. As our understanding of liver diseases evolves and expands, so too does our ability to mitigate risks and improve overall health outcomes, underscoring the importance of prioritizing liver wellness in our lives.