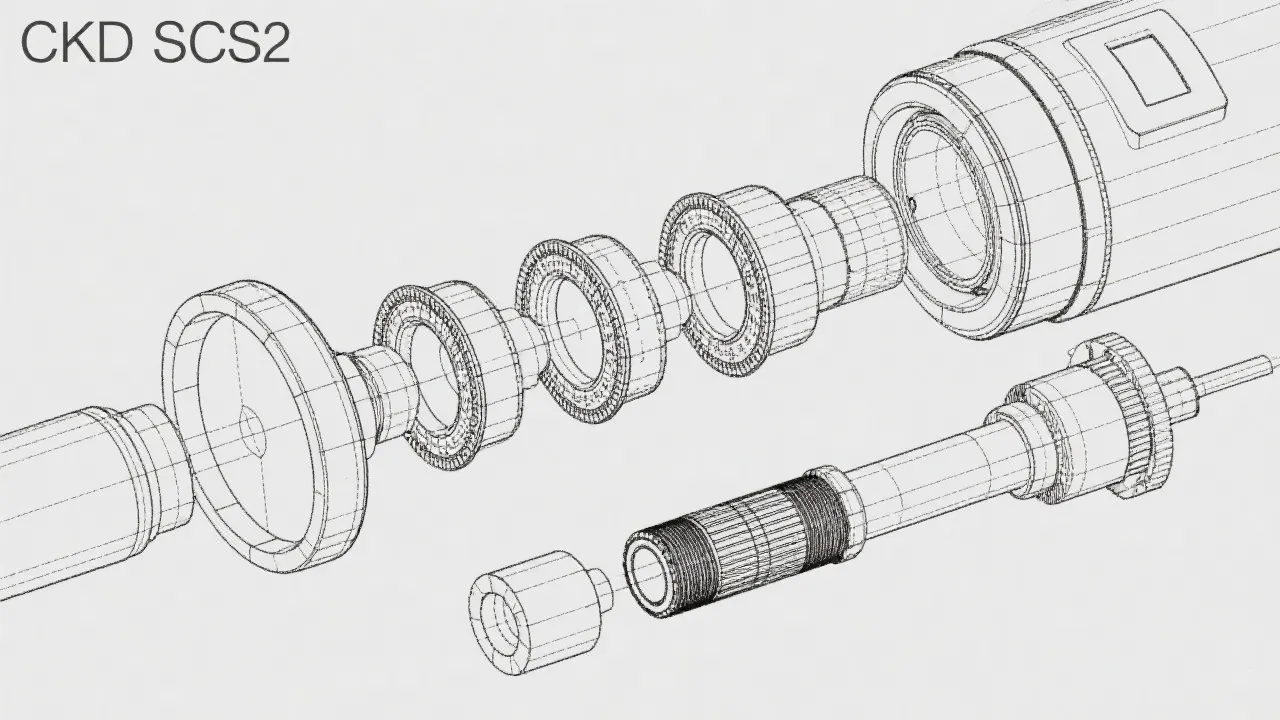
Understanding CKD SCS2 Technology
CKD SCS2 is at the forefront of advancements in kidney diagnostics, offering new insights into chronic kidney disease (CKD). As the global prevalence of CKD rises, technologies like CKD SCS2 become crucial for early detection and management. This article delves into its significance, applications, and the trajectory of kidney health management technologies.

Revolutionizing Kidney Health: CKD SCS2
Chronic Kidney Disease (CKD) is a growing global health challenge, with millions affected worldwide. CKD is characterized by a gradual loss of kidney function, which can lead to end-stage kidney disease and necessitates dialysis or kidney transplantation. It is a silent disease often undetected until it has advanced significantly. Advances in medical technology such as the CKD SCS2 play a vital role in addressing this issue by providing innovative solutions in detection and management. CKD SCS2 technology represents a significant leap forward in understanding and diagnosing CKD, offering healthcare professionals a more precise and comprehensive toolset to tackle this condition. This growing capability enhances both early detection and ongoing management, ultimately aiming to improve the quality of life for patients suffering from this chronic illness.
The Scope of CKD SCS2
The CKD SCS2 technology hinges on enhancing the capabilities of current diagnostic systems, focusing on improving the accuracy and efficiency of kidney function assessments. It integrates advanced biomarkers with traditional measures, offering clinicians a multidimensional view of kidney health. This approach not only aids early detection but also facilitates ongoing monitoring of disease progression or remission. For example, CKD SCS2 can help identify subtle changes in kidney function that may indicate developing issues long before they are evident through traditional measures alone. By combining data analytics and robust biochemistry, CKD SCS2 assists in the early identification of risk factors and the potential to mitigate CKD outcomes through timely intervention.
Industry Impacts and Developments
The implementation of CKD SCS2 technology has had significant impacts across the healthcare industry. By enhancing diagnostic accuracy, healthcare systems can reduce misdiagnoses and the corresponding potential mistreatment. Not only does this improve patient outcomes, but it also reduces unnecessary healthcare costs, aligning with the goals of value-based healthcare models increasingly adopted globally. The ability to provide accurate diagnoses allows for more targeted and efficient allocation of resources, reducing the burden on healthcare systems. Additionally, as healthcare providers recognize the value of CKD SCS2 in improving patient outcomes, there may be a shift towards preventative care models, focusing on maintaining kidney health rather than solely treating the disease after significant damage has occurred. This paradigm shift emphasizes proactive monitoring and individualized patient care, which can substantially drive better public health outcomes.
Enhancing Patient Outcomes with CKD SCS2
Using CKD SCS2 can result in a more personalized treatment plan for individuals diagnosed with CKD. By providing detailed insights into the specific functioning of a patient's kidneys, treatments can be better tailored to meet individual needs, ultimately enhancing the effectiveness of clinical interventions. For instance, CKD SCS2 allows for stratification of risk based on individual patient data, which helps determine the most appropriate therapeutic approaches—whether pharmacological, lifestyle modifications, or interdisciplinary referrals to dietitians and nephrologists. Moreover, enhanced patient engagement is facilitated as they can comprehend their health status through clearer and more comprehensive information presented by healthcare providers. This collaborative approach not only empowers patients but also fosters adherence to treatment protocols and lifestyle changes that can significantly slow disease progression.
Challenges and Considerations
Despite its benefits, the adoption of CKD SCS2 is not without challenges. The complexity and cost of implementing such advanced diagnostic technology can be barriers in widespread deployment, particularly in resource-limited settings. Healthcare facilities, especially in low- and middle-income countries, may lack the required infrastructure or funding to support the integration of CKD SCS2 systems. Furthermore, the integration of these newer diagnostic systems with existing healthcare infrastructures necessitates careful planning and adaptation. Resistance to change from healthcare providers accustomed to traditional methods can also impede the adoption of such innovations. Ongoing education and training for medical personnel will be crucial in overcoming these hurdles, ensuring that staff is capable of utilizing CKD SCS2 technology effectively. Involving stakeholders from various sectors—including healthcare policymakers, industry leaders, and patient advocates—will also be necessary to create policies that support the equitable adoption of CKD SCS2 technology across different healthcare environments.
Comparative Analysis of CKD Monitoring Techniques
| Technique | Description |
|---|---|
| Traditional Biomarkers | Reliance on markers such as creatinine and albumin to assess kidney function. These markers are often limited in their ability to detect early changes in kidney health and may not accurately reflect the overall kidney health status. |
| CKD SCS2 Technology | Incorporates advanced biomarkers for a more comprehensive kidney health analysis, utilizing multi-faceted data that can reveal not only current kidney function but also potential risk factors for progression. This technology can detect minor changes that can indicate the onset of complications before they become severe. |
| Ultrasound | Non-invasive imaging to assess kidney structure and size, useful for identifying anatomical abnormalities but limited in assessing functional capacity. While ultrasound provides valuable information regarding kidney integrity, it cannot interpret metabolic processes or assess the biochemical processes underway in the kidneys. |
Looking Ahead: The Future of Kidney Diagnostics
As medical technologies continue to evolve, the potential of CKD SCS2 to revolutionize kidney diagnostics grows. Future research is likely to focus on enhancing the predictive capabilities of this technology further and integrating it with other emerging technologies such as artificial intelligence (AI) and machine learning to provide even greater diagnostic accuracy. By analyzing vast datasets collected from various populations, AI algorithms can identify patterns and predict kidney disease progression or response to treatment much more effectively than traditional methods alone. This synergy has the potential to streamline the clinical workflow and improve timely interventions, thereby further enhancing patient outcomes. Furthermore, as developments in telemedicine and remote patient monitoring expand, the utility of CKD SCS2 may increase by enabling nephrologists to assess patient health from afar, allowing for constant renal health monitoring in conjunction with personalized feedback for patients.
Conclusion
CKD SCS2 stands out as a promising advancement in the ongoing battle against chronic kidney disease. By offering a more nuanced understanding of kidney function, it enhances diagnostic precision, leading to better patient management strategies and outcomes. The multi-layered insights provided by CKD SCS2 not only refine clinical assessments but also open new horizons for research into the pathophysiology of CKD. As the healthcare landscape evolves, so too will the tools we use, and CKD SCS2 remains at the forefront of this transformation, potentially redefining the standards of kidney disease management for years to come. As awareness of CKD continues to increase, the implementation and support for advanced diagnostic technologies like CKD SCS2 will be critical in ultimately improving population health and mitigating the impact of this chronic illness on individuals and healthcare systems alike.
FAQs about CKD SCS2
- What is CKD SCS2? CKD SCS2 is an advanced diagnostic technology that offers comprehensive insights into kidney function by integrating both traditional and advanced biomarkers. This multifaceted approach allows healthcare providers to see a clearer and more complete picture of renal health.
- How does CKD SCS2 differ from traditional methods? Unlike traditional diagnostic methods, which primarily rely on a limited set of markers such as creatinine and albumin, CKD SCS2 provides a multidimensional view of kidney health, improving accuracy and aiding in personalized treatment plans. By utilizing advanced biomarkers, it can detect subtle changes in kidney health that traditional methods might miss.
- What are the challenges in implementing CKD SCS2? High costs and integration with existing diagnostics pose significant challenges, especially in resource-limited settings. Additionally, the complexity of the new systems may necessitate extensive training for healthcare providers, further complicating implementation.
- What is the future of CKD SCS2 technology? Future directions involve enhancing predictive capabilities and integration with AI and machine learning for even greater accuracy, as well as expanding use in telemedicine to enable more widespread monitoring and management of CKD patients throughout the continuum of care.
The Importance of Patient Education in CKD Management
Effective management of chronic kidney disease involves not just diagnostic technology, but also a strong emphasis on patient education. Empowering patients with knowledge about their condition can lead to improved management strategies and overall health outcomes. Education encompasses a variety of critical areas, including understanding the disease process, recognizing the importance of adhering to prescribed treatments, and making informed lifestyle choices that can positively impact kidney health.
One of the critical aspects of patient education is promoting awareness about the risk factors associated with CKD. Several factors can predispose individuals to developing kidney disease, including hypertension, diabetes, and a family history of kidney problems. Patients should be encouraged to monitor their blood pressure and blood sugar levels closely and understand the implications of these conditions on their kidney health. Education initiatives can also guide patients on recognizing the early signs of kidney damage or decline, such as changes in urination patterns, fatigue, and swelling in different parts of the body.
Furthermore, dietary considerations play a significant role in managing CKD. Patients should be educated about the importance of adhering to renal-friendly dietary guidelines, which may include restricting sodium, potassium, and phosphorus intake, as well as maintaining adequate hydration. Nutritionists and dietitians can collaborate with nephrologists to form comprehensive dietary plans tailored to individual patient needs, which can significantly enhance patient outcomes.
The Role of Technology in Patient Engagement
In the modern era, technology serves as a potent tool for enhancing patient engagement in the management of CKD. Mobile applications and online platforms can be utilized to promote self-management, track health metrics, and facilitate communication between patients and healthcare providers. Telehealth solutions allow patients to have regular consultations and follow-ups with their healthcare providers without the burden of travel, which can be particularly beneficial for those living in remote areas or with mobility issues.
Moreover, wearable technology is emerging as a valuable asset in kidney disease management. Devices that monitor vital signs, physical activity, and even hydration levels can provide real-time feedback to patients and healthcare professionals, aligning well with the principles of personalized medicine. This proactive approach toward healthcare can significantly enhance patients’ adherence to treatment protocols and empower them to take charge of their own health.
Collaborative Care Models in CKD Management
A collaborative care model is essential for the successful management of CKD, leveraging the strengths of multifaceted healthcare teams to deliver comprehensive patient care. By engaging professionals from various disciplines, including nephrologists, primary care physicians, dietitians, nurses, and social workers, healthcare providers can create holistic treatment plans that address the physical, emotional, and financial challenges faced by patients.
Furthermore, leveraging community resources and support groups can greatly benefit patients by providing emotional support, shared experiences, and education. Patients with chronic diseases often report feelings of isolation and distress; hence, establishing a network of support is critical. Community-based education programs and support groups can empower patients and caregivers alike, enhancing discussions about treatment options, resources, and lifestyle modifications that can improve outcomes.
Policy Implications and Health Equity in CKD
The rising burden of CKD underscores the need for effective policy implications that address health disparities and promote equitable access to innovative diagnostic technologies like CKD SCS2. Policymakers must recognize the socio-economic factors contributing to the prevalence of kidney disease and create strategic frameworks that enhance screening efforts and care delivery in underserved communities. Initiatives aiming to reduce barriers, such as financial assistance programs, transportation services to healthcare facilities, and languages support, can greatly increase access to necessary healthcare services.
Moreover, increasing public awareness of CKD and its risk factors through community outreach programs can be vital in facilitating early intervention and prevention strategies. Public health campaigns promoting healthy lifestyles, disease screening, and educational initiatives focused on kidney health can help bridge the gap in education and access to care. By prioritizing health equity in CKD management, we can work towards reducing the burgeoning health disparities and improve overall health outcomes across diverse populations.